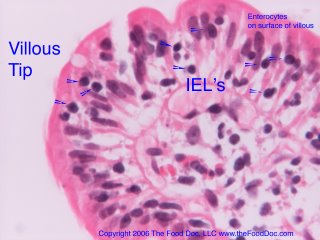
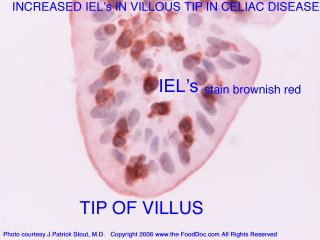
Out of the United Kingdom, comes a new article proposing that intraepithelial lymphocytes (IEL's) are important in maintaining the integrity of the tight junctions of gut to prevent the leaky gut syndrome. IEL’s are seen in increased numbers near the surface of the intestinal lining in a variety of abnormal intestinal conditions, most notably celiac disease. Being close to intestinal epithelial cells, IEL's are thought to perform several functions including tumor surveillance, restoration and repair of the lining, fighting infection, and according to new research, maintaining the tight junctions. This latter function is crucial to maintaining the gut barrier or preventing the leaky gut syndrome.
Dalton and co-investigators from the United Kingdom recently published date showing that in mice γδ+ intraepithelial lymphocytes help maintain the integrity of the epithelial cell barrier. Mice deficient in γδ+ IEL’s had severely compromised barrier function and were highly susceptible to infection from infections from Toxoplasma and Salmonella typhimurium. Reconstitution of IEL’s in deficient mice had restored intestinal barrier.
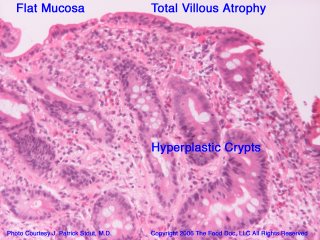
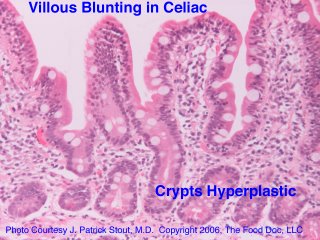
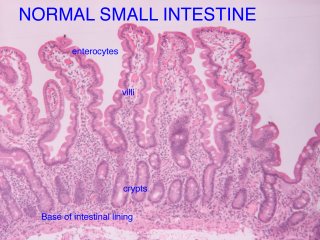
It is noteworthy that throughout the gastrointestinal tract there is only one layer of intestinal lining cells preventing what is foreign or toxic to you in what you eat or drink from gaining entry into your body. A long continuous single layer wall of epithelial cells, known as enterocytes in the small intestine, normally joined tightly, lines the entire gut. See my diagram of the intestinal villous and also my previous blogs on the intraepithelial lymphocytes. Excess IEL's are known to cause gut injury and thereby promote leaky gut, as in celiac disease.
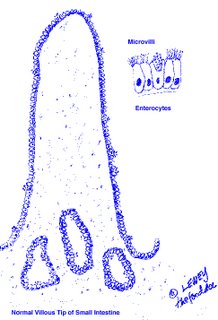
The single layer of epithelial cells are the entry point for water and nutrients while at same time acting as a barrier to foreign proteins such as bacteria, viruses, food proteins or lectins, and noxious chemicals or toxins present in what we eat or drink. In contrast to the gut, the skin, another barrier of the body to external invaders, has a multi-layer lining of epithelial cells, rather than a single layer.
Joined by tight junctions (TJ’s) through a sophisticated system of proteins, including occludin and a regulatory protein zonulin, the epithelial gut layer serves as a barrier to foreign proteins. When this barrier is breached, foreign proteins such as bacteria and intact food proteins or lectins, may gain entry into our bodies and cause disease. Various injuries gut can result in gaps by loosening up the tight junctions (TJ’s) between the intestinal lining cells. What results is effectively a leaky gut.
How important is preventing the leaky gut syndrome? Dalton and co-workers make this statement in their discussion of their findings about the importance of IEL’s maintaining the TJ’s. “Diseases including cancer, diarrhea, inflammatory bowel disease, multiple sclerosis, diabetes, and allergic disorders are associated with disruption of TJ’s and alterations in the regulation of occludin”.
Earlier in their article they use the term “leaky” TJ complexes to describe how bacteria could infect mice deficient in the IEL’s necessary to maintain gut integrity. This article furthers our understanding on how the gut barrier is maintained and may be injured. The concept of the leaky gut as an entry way to the body for infection, toxins, and foreign food proteins resulting in infection, toxicity and/or autoimmune disease(s) continues to intrigue those of who are interested and who have eyes to see. To receive regular updates as I continue to follow important research you may subscribe to this blog by clicking on the atom feed.
Reference:
Dalton, JE et.al., Intraepithelial γδ+ lymphocytes maintain integrity of the intestinal epithelial tight junctions in response to infection. Gastroenterology 2006;131:818-829.
Copyright © 2006, The Food Doc, LLC. All Rights Reserved. www.thefooddoc.com